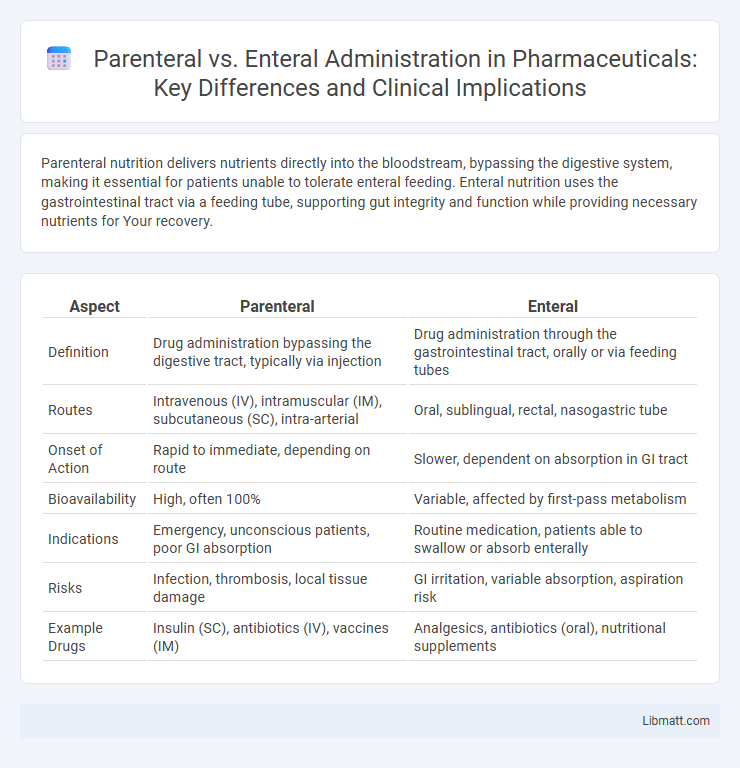
Parenteral nutrition delivers nutrients directly into the bloodstream, bypassing the digestive system, making it essential for patients unable to tolerate enteral feeding. Enteral nutrition uses the gastrointestinal tract via a feeding tube, supporting gut integrity and function while providing necessary nutrients for Your recovery.
Table of Comparison
| Aspect | Parenteral | Enteral |
|---|---|---|
| Definition | Drug administration bypassing the digestive tract, typically via injection | Drug administration through the gastrointestinal tract, orally or via feeding tubes |
| Routes | Intravenous (IV), intramuscular (IM), subcutaneous (SC), intra-arterial | Oral, sublingual, rectal, nasogastric tube |
| Onset of Action | Rapid to immediate, depending on route | Slower, dependent on absorption in GI tract |
| Bioavailability | High, often 100% | Variable, affected by first-pass metabolism |
| Indications | Emergency, unconscious patients, poor GI absorption | Routine medication, patients able to swallow or absorb enterally |
| Risks | Infection, thrombosis, local tissue damage | GI irritation, variable absorption, aspiration risk |
| Example Drugs | Insulin (SC), antibiotics (IV), vaccines (IM) | Analgesics, antibiotics (oral), nutritional supplements |
Introduction to Parenteral and Enteral Nutrition
Parenteral nutrition delivers nutrients directly into the bloodstream through intravenous therapy, bypassing the digestive system entirely. Enteral nutrition involves feeding through a tube placed in the gastrointestinal tract, supporting natural digestive processes. Understanding the differences between parenteral and enteral nutrition helps you choose the optimal method for patients who cannot meet their nutritional needs orally.
Definitions and Key Differences
Parenteral nutrition involves delivering nutrients directly into the bloodstream via intravenous methods, bypassing the digestive system, and is essential for patients with non-functional gastrointestinal tracts. Enteral nutrition delivers nutrients through the digestive tract, usually via oral or tube feeding, maintaining gut integrity and reducing infection risks. Key differences include the route of administration, physiological impact on the digestive system, and associated complications such as infection risk with parenteral access versus gastrointestinal tolerance with enteral feeding.
Indications for Parenteral Nutrition
Parenteral nutrition is indicated when the gastrointestinal tract is non-functional or inaccessible due to conditions such as severe pancreatitis, bowel obstruction, short bowel syndrome, or critical illness impairing nutrient absorption. It is essential for patients who cannot meet their nutritional needs via enteral routes despite attempts at oral or tube feeding. This approach provides complete nutrient delivery intravenously, ensuring adequate caloric and micronutrient support in complex clinical scenarios.
Indications for Enteral Nutrition
Enteral nutrition is indicated for patients with a functional gastrointestinal tract who cannot meet their nutritional needs orally due to conditions such as stroke, traumatic brain injury, or critical illness. It supports gut integrity and reduces the risk of infections compared to parenteral nutrition. Your healthcare provider will recommend enteral feeding when oral intake is insufficient but the digestive system remains operational.
Advantages of Parenteral Nutrition
Parenteral nutrition offers the advantage of delivering essential nutrients directly into the bloodstream, bypassing the digestive system, which is crucial for patients with compromised gastrointestinal function or absorption issues. It ensures precise control over nutrient composition tailored to individual metabolic needs, supporting recovery in critical care, malnutrition, or severe gastrointestinal disorders. This method also reduces the risk of gastrointestinal complications such as paralytic ileus, bowel obstruction, or infections related to enteral feeding tubes.
Advantages of Enteral Nutrition
Enteral nutrition supports gut integrity by maintaining mucosal structure and function, which reduces the risk of bacterial translocation and infection. It is cost-effective and associated with fewer complications compared to parenteral nutrition, such as catheter-related bloodstream infections. Enteral feeding also promotes better nutrient absorption and preserves the normal digestive process, enhancing overall patient outcomes.
Risks and Complications of Parenteral Nutrition
Parenteral nutrition carries significant risks such as bloodstream infections, thrombosis, and metabolic complications including hyperglycemia and electrolyte imbalances. Catheter-related issues like occlusion or mechanical injury pose further threats, requiring vigilant monitoring. Your healthcare team must weigh these potential complications against the benefits when considering parenteral nutrition for optimal patient outcomes.
Risks and Complications of Enteral Nutrition
Enteral nutrition carries risks such as aspiration pneumonia, tube displacement, and gastrointestinal issues like diarrhea or constipation. Infection at the insertion site and metabolic complications, including electrolyte imbalances, can also occur with enteral feeding. You should closely monitor for these complications to ensure safe and effective nutritional support.
Clinical Decision Criteria: Choosing the Right Method
Clinical decision criteria for choosing parenteral versus enteral nutrition hinge on gastrointestinal function, patient risk factors, and nutritional goals. Parenteral nutrition is indicated when the gastrointestinal tract is non-functional or inaccessible, while enteral nutrition is preferred for patients with a functional gut to maintain mucosal integrity and minimize infection risk. Your healthcare team evaluates factors like severity of malnutrition, risk of aspiration, and metabolic requirements to determine the optimal feeding method.
Conclusion and Future Perspectives
Parenteral nutrition provides critical support for patients unable to utilize their gastrointestinal tract, delivering essential nutrients intravenously. Enteral nutrition, using the digestive system, remains preferred due to lower infection risks and better preservation of gut integrity. Future perspectives emphasize personalized nutrition strategies, advanced formulations, and integration of biomarkers to optimize patient outcomes and minimize complications in both modalities.
Parenteral vs enteral Infographic
 libmatt.com
libmatt.com