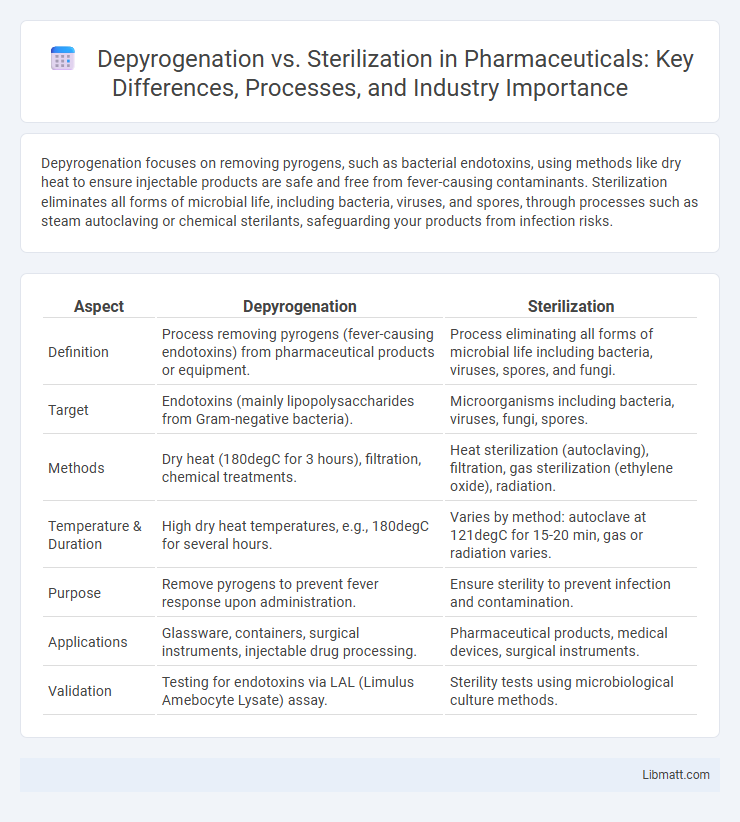
Depyrogenation focuses on removing pyrogens, such as bacterial endotoxins, using methods like dry heat to ensure injectable products are safe and free from fever-causing contaminants. Sterilization eliminates all forms of microbial life, including bacteria, viruses, and spores, through processes such as steam autoclaving or chemical sterilants, safeguarding your products from infection risks.
Table of Comparison
| Aspect | Depyrogenation | Sterilization |
|---|---|---|
| Definition | Process removing pyrogens (fever-causing endotoxins) from pharmaceutical products or equipment. | Process eliminating all forms of microbial life including bacteria, viruses, spores, and fungi. |
| Target | Endotoxins (mainly lipopolysaccharides from Gram-negative bacteria). | Microorganisms including bacteria, viruses, fungi, spores. |
| Methods | Dry heat (180degC for 3 hours), filtration, chemical treatments. | Heat sterilization (autoclaving), filtration, gas sterilization (ethylene oxide), radiation. |
| Temperature & Duration | High dry heat temperatures, e.g., 180degC for several hours. | Varies by method: autoclave at 121degC for 15-20 min, gas or radiation varies. |
| Purpose | Remove pyrogens to prevent fever response upon administration. | Ensure sterility to prevent infection and contamination. |
| Applications | Glassware, containers, surgical instruments, injectable drug processing. | Pharmaceutical products, medical devices, surgical instruments. |
| Validation | Testing for endotoxins via LAL (Limulus Amebocyte Lysate) assay. | Sterility tests using microbiological culture methods. |
Understanding Depyrogenation and Sterilization
Depyrogenation and sterilization are critical processes in pharmaceutical and medical device manufacturing, each targeting different contaminants; depyrogenation specifically removes pyrogens such as endotoxins through methods like dry heat or chemical treatment, while sterilization eliminates all forms of microbial life using techniques such as steam autoclaving or radiation. Understanding the distinction is essential for ensuring product safety, as pyrogens can cause severe immune reactions even in sterile products. Effective depyrogenation complements sterilization by addressing microbial toxins that standard sterilization processes may not eliminate.
Key Differences Between Depyrogenation and Sterilization
Depyrogenation removes heat-resistant pyrogens, such as endotoxins, from medical equipment and pharmaceutical products, ensuring they are safe for injection and intravenous use. Sterilization eliminates all forms of microbial life, including bacteria, viruses, fungi, and spores, to prevent infection and contamination. Understanding these key differences helps you choose the appropriate process for ensuring product safety and compliance with regulatory standards.
Importance in Pharmaceutical Manufacturing
Depyrogenation and sterilization are critical processes in pharmaceutical manufacturing to ensure product safety and efficacy. Depyrogenation removes pyrogens, particularly endotoxins from bacterial cell walls, preventing fever-inducing contaminants in injectable drugs. Sterilization eliminates all forms of microbial life, including bacteria, viruses, and spores, safeguarding sterile pharmaceuticals from infection risks.
Mechanisms of Depyrogenation
Depyrogenation primarily involves the removal or destruction of pyrogens, such as bacterial endotoxins, through methods like dry heat treatment at temperatures above 250degC, which denatures and breaks down lipopolysaccharide molecules. This process differs from sterilization that targets the complete elimination of all viable microorganisms, including bacteria, viruses, and spores. Effective depyrogenation relies on thermal destruction mechanisms that ensure endotoxins are rendered non-toxic without necessarily sterilizing the product.
Mechanisms of Sterilization
Sterilization eliminates all forms of microbial life through physical or chemical methods such as autoclaving, dry heat, or chemical sterilants that disrupt cellular structures and functions. Mechanisms include protein denaturation, membrane disruption, and nucleic acid damage, effectively inactivating bacteria, viruses, fungi, and spores. Autoclaving uses pressurized steam to achieve thermal denaturation of proteins, while chemical sterilants like ethylene oxide alkylate nucleic acids to prevent replication.
Common Methods of Depyrogenation
Depyrogenation commonly involves dry heat, which effectively destroys pyrogens by exposure to temperatures between 160degC and 250degC for specific durations. Another method includes depyrogenation by chemical means, such as alkaline hydrolysis, which breaks down endotoxins on equipment surfaces. Understanding these methods helps ensure your pharmaceutical or medical products meet safety standards by removing harmful pyrogens prior to sterilization.
Common Sterilization Techniques
Common sterilization techniques include autoclaving, dry heat sterilization, ethylene oxide gas, and radiation, each targeting microbial inactivation through different mechanisms. Autoclaving uses steam under pressure to denature proteins and destroy microorganisms, while dry heat sterilization oxidizes cellular components at high temperatures for extended periods. Ethylene oxide gas sterilizes by alkylating DNA and proteins, effective for heat-sensitive materials, and radiation sterilization employs gamma rays or electron beams to break genetic material, ensuring microbial destruction.
Regulatory Guidelines and Standards
Regulatory guidelines for depyrogenation and sterilization are critical in ensuring product safety in pharmaceutical manufacturing, governed by agencies like the FDA and EMA. Depyrogenation standards focus on eliminating endotoxins, following USP <85> and EP 2.6.14, while sterilization adheres to sterility assurance levels outlined in ISO 11137 and USP <71>. Your compliance with these specific guidelines ensures both processes meet the required safety and efficacy standards for sterile drug products.
Challenges and Limitations
Depyrogenation faces challenges such as the need for extremely high temperatures or chemical treatments to effectively remove endotoxins without damaging sensitive equipment or materials. Sterilization can be limited by the resistance of certain microorganisms and the potential degradation of heat-sensitive products during processes like autoclaving or gamma irradiation. Both methods require careful validation to ensure efficacy while maintaining product integrity and compliance with regulatory standards.
Choosing the Right Method for Your Application
Selecting the appropriate method between depyrogenation and sterilization depends on the nature of the contaminants and the intended application. Depyrogenation effectively removes pyrogens such as bacterial endotoxins from medical equipment and pharmaceuticals, ensuring safety in injections. Sterilization targets the destruction of all microbial life, including bacteria, viruses, and spores, making it essential for surgical instruments and sterile environments in healthcare settings.
Depyrogenation vs Sterilization Infographic
 libmatt.com
libmatt.com