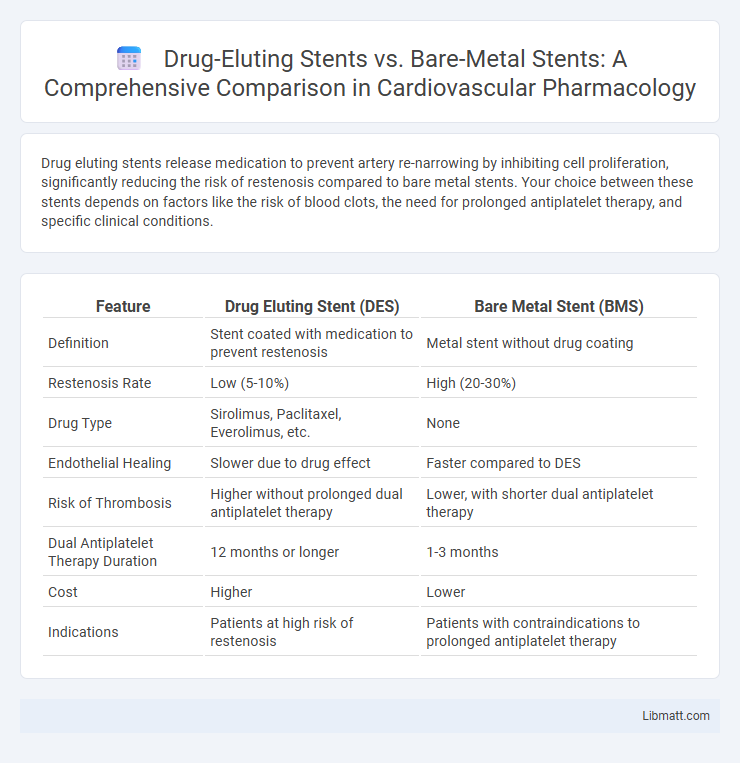
Drug eluting stents release medication to prevent artery re-narrowing by inhibiting cell proliferation, significantly reducing the risk of restenosis compared to bare metal stents. Your choice between these stents depends on factors like the risk of blood clots, the need for prolonged antiplatelet therapy, and specific clinical conditions.
Table of Comparison
| Feature | Drug Eluting Stent (DES) | Bare Metal Stent (BMS) |
|---|---|---|
| Definition | Stent coated with medication to prevent restenosis | Metal stent without drug coating |
| Restenosis Rate | Low (5-10%) | High (20-30%) |
| Drug Type | Sirolimus, Paclitaxel, Everolimus, etc. | None |
| Endothelial Healing | Slower due to drug effect | Faster compared to DES |
| Risk of Thrombosis | Higher without prolonged dual antiplatelet therapy | Lower, with shorter dual antiplatelet therapy |
| Dual Antiplatelet Therapy Duration | 12 months or longer | 1-3 months |
| Cost | Higher | Lower |
| Indications | Patients at high risk of restenosis | Patients with contraindications to prolonged antiplatelet therapy |
Introduction to Coronary Stents
Coronary stents are small, mesh-like tubes inserted into narrowed or blocked coronary arteries to restore blood flow and prevent artery collapse. Drug-eluting stents (DES) release medication that inhibits cell proliferation, reducing the risk of restenosis compared to Bare Metal Stents (BMS), which lack such coating and have higher rates of artery re-narrowing. Your choice between DES and BMS can impact long-term artery health and the need for prolonged antiplatelet therapy.
Overview of Bare Metal Stents (BMS)
Bare Metal Stents (BMS) are metallic mesh tubes implanted into coronary arteries to maintain vessel patency after angioplasty. They provide structural support but have a higher risk of restenosis due to neointimal hyperplasia. BMS are typically preferred in patients with contraindications to prolonged dual antiplatelet therapy or in settings requiring shorter anticoagulation duration.
Evolution and Technology of Drug Eluting Stents (DES)
Drug Eluting Stents (DES) represent a significant technological advancement over Bare Metal Stents (BMS) by releasing antiproliferative drugs that reduce the risk of restenosis and promote better long-term arterial healing. Modern DES utilize biocompatible polymer coatings and second-generation drugs, improving safety profiles and minimizing inflammation compared to earlier models. Understanding the evolution from BMS to DES can help you make informed decisions about coronary artery disease treatments optimized for reduced revascularization rates and enhanced vessel patency.
Mechanism of Action: BMS vs DES
Bare metal stents (BMS) act as a scaffold to keep the artery open but lack drug delivery, which often leads to neointimal hyperplasia and restenosis. Drug-eluting stents (DES) release antiproliferative medications such as sirolimus or paclitaxel, inhibiting smooth muscle cell proliferation and significantly reducing restenosis rates. This targeted drug release mechanism in DES improves long-term patency compared to BMS by minimizing vessel re-narrowing after implantation.
Clinical Indications and Patient Selection
Drug eluting stents (DES) are primarily indicated for patients with high risk of restenosis, such as those with diabetes, long or complex coronary lesions, and small vessel disease, offering improved outcomes by releasing antiproliferative drugs that reduce neointimal hyperplasia. Bare metal stents (BMS) may be preferred in patients with high bleeding risk who require shorter duration of dual antiplatelet therapy or those with simpler lesion profiles where restenosis risk is lower. Your clinical decision should consider factors like patient comorbidities, lesion characteristics, and the need for long-term antiplatelet therapy to optimize stent selection.
Efficacy and Safety Outcomes
Drug eluting stents (DES) demonstrate superior efficacy in reducing restenosis rates and target lesion revascularization compared to bare metal stents (BMS). Safety outcomes reveal a lower incidence of in-stent restenosis and repeat interventions with DES, though concerns about late stent thrombosis necessitate prolonged dual antiplatelet therapy. Clinical trials consistently show DES improve long-term vessel patency while maintaining an acceptable safety profile relative to BMS.
Risk of Restenosis: A Comparative Analysis
Drug eluting stents (DES) significantly reduce the risk of restenosis compared to bare metal stents (BMS) by releasing antiproliferative drugs that inhibit neointimal hyperplasia. Clinical studies demonstrate restenosis rates of approximately 5-10% in DES recipients versus 20-30% with BMS within the first year post-implantation. This reduction in restenosis with DES leads to lower rates of repeat revascularization and improved long-term vessel patency.
Long-term Complications and Considerations
Drug eluting stents (DES) significantly reduce the risk of in-stent restenosis compared to bare metal stents (BMS) by releasing antiproliferative drugs that inhibit neointimal hyperplasia. However, DES are associated with a higher risk of late stent thrombosis, necessitating prolonged dual antiplatelet therapy to prevent adverse events. Long-term considerations include balancing the reduced restenosis rates of DES against the potential bleeding risks from extended antiplatelet use, whereas BMS may require repeat revascularization due to higher restenosis rates.
Cost-effectiveness and Healthcare Impact
Drug-eluting stents (DES) offer superior efficacy by reducing restenosis rates compared to bare-metal stents (BMS), which often leads to fewer repeat procedures and lower long-term healthcare costs. Although the initial cost of DES is higher, their improved outcomes contribute to better cost-effectiveness and reduced hospitalization expenses in your cardiovascular care. Healthcare systems benefit from decreased complication rates and improved patient quality of life by prioritizing DES in appropriate clinical scenarios.
Future Trends in Stent Development and Usage
Future trends in stent development emphasize bioresorbable scaffolds and advanced drug-eluting technologies to reduce restenosis and improve long-term vessel healing. Innovations in polymer coatings and personalized drug delivery systems aim to optimize patient outcomes by minimizing inflammation and thrombosis risks. You can expect increased adoption of smart stents with embedded sensors to monitor vascular health in real-time, enhancing post-implantation care.
Drug eluting stent vs Bare metal stent Infographic
 libmatt.com
libmatt.com