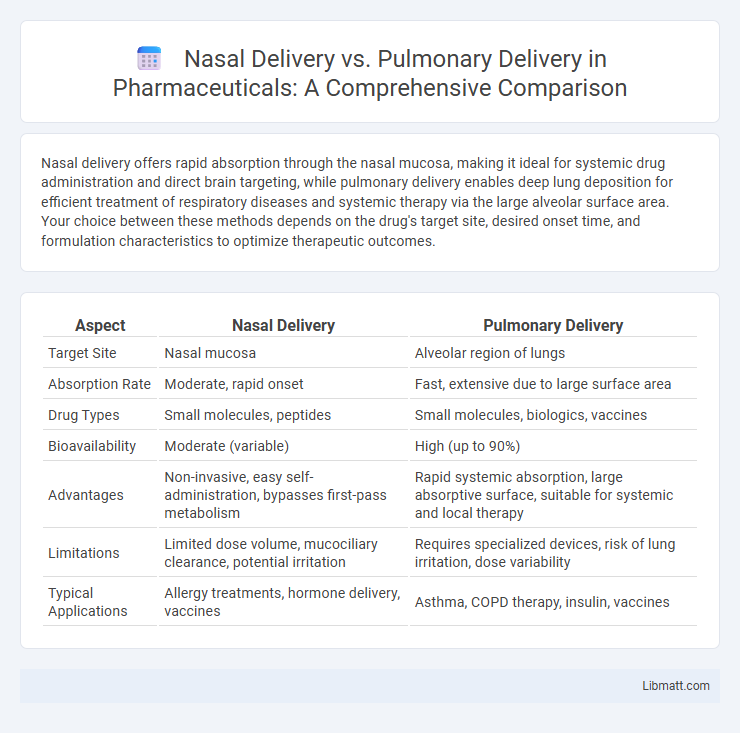
Nasal delivery offers rapid absorption through the nasal mucosa, making it ideal for systemic drug administration and direct brain targeting, while pulmonary delivery enables deep lung deposition for efficient treatment of respiratory diseases and systemic therapy via the large alveolar surface area. Your choice between these methods depends on the drug's target site, desired onset time, and formulation characteristics to optimize therapeutic outcomes.
Table of Comparison
| Aspect | Nasal Delivery | Pulmonary Delivery |
|---|---|---|
| Target Site | Nasal mucosa | Alveolar region of lungs |
| Absorption Rate | Moderate, rapid onset | Fast, extensive due to large surface area |
| Drug Types | Small molecules, peptides | Small molecules, biologics, vaccines |
| Bioavailability | Moderate (variable) | High (up to 90%) |
| Advantages | Non-invasive, easy self-administration, bypasses first-pass metabolism | Rapid systemic absorption, large absorptive surface, suitable for systemic and local therapy |
| Limitations | Limited dose volume, mucociliary clearance, potential irritation | Requires specialized devices, risk of lung irritation, dose variability |
| Typical Applications | Allergy treatments, hormone delivery, vaccines | Asthma, COPD therapy, insulin, vaccines |
Introduction to Nasal and Pulmonary Drug Delivery
Nasal drug delivery utilizes the rich vascularization and large surface area of the nasal mucosa for rapid drug absorption and onset of action, making it ideal for systemic and local treatments. Pulmonary drug delivery targets the extensive alveolar surface within the lungs to enable efficient absorption of drugs, particularly for respiratory conditions and systemic therapies requiring fast bioavailability. Both routes offer non-invasive alternatives to oral and injectable administration, with unique advantages based on anatomical and physiological characteristics.
Mechanisms of Nasal Drug Absorption
Nasal drug absorption primarily occurs through the highly vascularized respiratory epithelium, enabling rapid systemic uptake via passive diffusion and active transport mechanisms. The presence of tight junctions and mucociliary clearance influences drug residence time and bioavailability, while enzymatic activity in the nasal mucosa can lead to pre-systemic drug metabolism. Compared to pulmonary delivery, nasal absorption offers a non-invasive route with potential for direct nose-to-brain transport through the olfactory region, bypassing the blood-brain barrier.
Mechanisms of Pulmonary Drug Absorption
Pulmonary drug absorption occurs primarily through the alveolar epithelium, where a large surface area and thin membrane facilitate rapid drug transfer into the bloodstream. The process involves drug dissolution in the lung lining fluid, followed by passive diffusion across epithelial cells or uptake via active transport mechanisms. You benefit from this efficient pathway when using inhalation therapies, as drugs can achieve quick systemic effects and enhanced bioavailability compared to nasal delivery.
Key Advantages of Nasal Delivery
Nasal delivery offers rapid drug absorption due to the rich vascularization of the nasal mucosa, enabling quick onset of action for treatments. This route bypasses the gastrointestinal tract and first-pass metabolism, enhancing bioavailability and reducing systemic side effects. Your therapies benefit from non-invasive administration and improved patient compliance, especially for drugs targeting the central nervous system.
Key Advantages of Pulmonary Delivery
Pulmonary delivery offers rapid systemic absorption due to the large surface area and thin alveolar membrane, enabling efficient drug transfer into the bloodstream. It bypasses first-pass metabolism, enhancing bioavailability and allowing for lower drug doses and reduced systemic side effects. This route is particularly advantageous for delivering drugs that require fast onset of action, such as for asthma, COPD, and systemic therapies via inhalation.
Limitations and Challenges of Nasal Delivery
Nasal delivery faces limitations such as restricted absorption surface area and mucociliary clearance, which significantly reduce drug residence time and bioavailability. The nasal epithelium's enzymatic activity also poses a challenge by degrading sensitive molecules before systemic absorption occurs. Furthermore, formulation constraints and variability in nasal anatomy among patients can impact the consistency and efficacy of nasal drug delivery.
Limitations and Challenges of Pulmonary Delivery
Pulmonary delivery faces significant limitations such as variable drug deposition due to particle size, airway anatomy, and breathing patterns, which affect therapeutic efficacy. Challenges include mucociliary clearance, enzymatic degradation in the lungs, and potential irritation or inflammation caused by the inhaled substances. Moreover, formulation stability and device design complexities pose hurdles in achieving consistent and targeted drug delivery to the pulmonary system.
Comparative Efficacy in Systemic Drug Delivery
Nasal delivery offers rapid absorption through the highly vascularized nasal mucosa, allowing efficient systemic drug uptake with bypass of first-pass metabolism, enhancing bioavailability for certain peptides and small molecules. Pulmonary delivery provides an extensive alveolar surface area and thin epithelial barrier facilitating quick systemic absorption of larger molecules and gases, often achieving higher drug bioavailability and faster onset of action. Comparative efficacy depends on drug properties, with pulmonary delivery generally superior for large molecule biologics, while nasal delivery suits smaller, lipophilic drugs requiring non-invasive systemic administration.
Clinical Applications and Use Cases
Nasal delivery is primarily utilized for rapid systemic drug absorption and treatment of local nasal conditions such as allergic rhinitis and sinusitis, offering non-invasive administration with quick onset. Pulmonary delivery targets the respiratory tract for direct treatment of lung diseases like asthma, chronic obstructive pulmonary disease (COPD), and cystic fibrosis, utilizing devices like inhalers and nebulizers to deliver medications deeply into the lungs. Both methods are critical in clinical settings but differ in targeting systemic circulation versus localized pulmonary therapy, influencing drug formulation and delivery device design.
Future Trends in Nasal vs Pulmonary Drug Delivery
Future trends in nasal drug delivery emphasize targeted therapies for central nervous system disorders through enhanced mucosal absorption and nanoparticle carriers. Pulmonary delivery advancements prioritize precision inhalers and smart devices that optimize drug deposition in the lower respiratory tract for chronic lung diseases. Integration of digital health technologies and personalized medicine is expected to drive innovation in both nasal and pulmonary drug delivery systems.
Nasal delivery vs Pulmonary delivery Infographic
 libmatt.com
libmatt.com