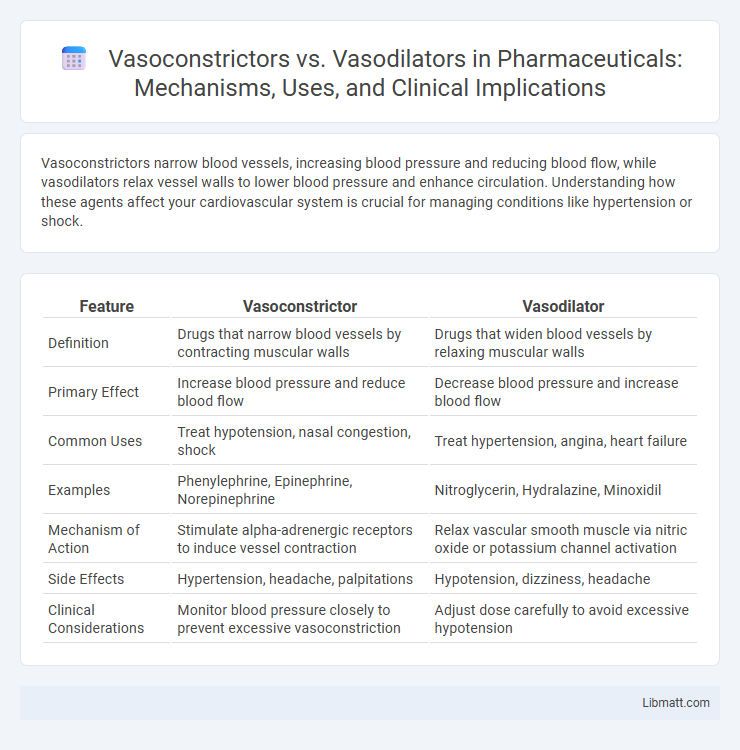
Vasoconstrictors narrow blood vessels, increasing blood pressure and reducing blood flow, while vasodilators relax vessel walls to lower blood pressure and enhance circulation. Understanding how these agents affect your cardiovascular system is crucial for managing conditions like hypertension or shock.
Table of Comparison
| Feature | Vasoconstrictor | Vasodilator |
|---|---|---|
| Definition | Drugs that narrow blood vessels by contracting muscular walls | Drugs that widen blood vessels by relaxing muscular walls |
| Primary Effect | Increase blood pressure and reduce blood flow | Decrease blood pressure and increase blood flow |
| Common Uses | Treat hypotension, nasal congestion, shock | Treat hypertension, angina, heart failure |
| Examples | Phenylephrine, Epinephrine, Norepinephrine | Nitroglycerin, Hydralazine, Minoxidil |
| Mechanism of Action | Stimulate alpha-adrenergic receptors to induce vessel contraction | Relax vascular smooth muscle via nitric oxide or potassium channel activation |
| Side Effects | Hypertension, headache, palpitations | Hypotension, dizziness, headache |
| Clinical Considerations | Monitor blood pressure closely to prevent excessive vasoconstriction | Adjust dose carefully to avoid excessive hypotension |
Introduction to Vasoconstrictors and Vasodilators
Vasoconstrictors are agents that narrow blood vessels by inducing the contraction of vascular smooth muscle, leading to increased blood pressure and reduced blood flow. Vasodilators, in contrast, relax these muscles, causing blood vessels to widen, which decreases blood pressure and enhances blood flow. Understanding the mechanisms of vasoconstrictors and vasodilators is essential for managing cardiovascular conditions such as hypertension and shock.
Defining Vasoconstrictors: Mechanism and Effects
Vasoconstrictors are agents that narrow blood vessels by stimulating the contraction of smooth muscle cells in the vessel walls, reducing blood flow and increasing blood pressure. Common vasoconstrictors include norepinephrine, epinephrine, and angiotensin II, which activate alpha-adrenergic receptors to trigger vessel constriction. Understanding the mechanism of vasoconstrictors helps you manage conditions like hypertension and shock by modulating vascular resistance effectively.
Understanding Vasodilators: Mechanism and Effects
Vasodilators work by relaxing the smooth muscles in blood vessel walls, leading to the widening of arteries and veins. This process decreases vascular resistance and increases blood flow, which helps reduce blood pressure and improves oxygen delivery to tissues. Understanding the mechanism of vasodilators allows you to appreciate their therapeutic role in treating conditions such as hypertension, heart failure, and angina.
Key Differences Between Vasoconstrictors and Vasodilators
Vasoconstrictors narrow blood vessels by stimulating smooth muscle contraction, leading to increased blood pressure and reduced blood flow; common examples include norepinephrine and phenylephrine. Vasodilators relax vascular smooth muscles, causing vessel dilation, decreased blood pressure, and enhanced blood flow, with drugs like nitroglycerin and hydralazine serving as typical agents. The key difference lies in their opposing effects on vascular tone--vasoconstrictors raise vascular resistance, while vasodilators lower it, directly impacting cardiovascular dynamics and therapeutic uses.
Common Types and Examples of Vasoconstrictors
Common vasoconstrictors include norepinephrine, epinephrine, and phenylephrine, all of which act on alpha-adrenergic receptors to narrow blood vessels and increase blood pressure. Other notable vasoconstrictors are vasopressin and angiotensin II, which regulate vascular tone and fluid balance. These agents are commonly used in clinical settings to treat hypotension, shock, and nasal congestion.
Common Types and Examples of Vasodilators
Common types of vasodilators include nitrates, calcium channel blockers, and angiotensin-converting enzyme (ACE) inhibitors, which are frequently used to treat hypertension and heart failure. Examples like nitroglycerin, amlodipine, and enalapril effectively relax blood vessels by targeting smooth muscle cells, improving blood flow and reducing vascular resistance. These vasodilators play a critical role in managing cardiovascular conditions by lowering blood pressure and enhancing oxygen delivery.
Medical Uses and Indications of Vasoconstrictors
Vasoconstrictors are primarily used in medical settings to manage hypotension during anesthesia, control bleeding in surgeries, and treat nasal congestion by narrowing blood vessels to reduce blood flow. They are indicated for preventing shock in trauma patients and managing conditions like migraines through targeted vasoconstriction. Common vasoconstrictors include epinephrine, phenylephrine, and norepinephrine, each utilized for their rapid effect in stabilizing blood pressure and reducing hemorrhage.
Therapeutic Applications of Vasodilators
Vasodilators, such as nitrates, calcium channel blockers, and ACE inhibitors, are primarily used to treat hypertension, heart failure, and angina by relaxing blood vessels and improving blood flow. These medications reduce vascular resistance and myocardial oxygen demand, enhancing cardiac output and alleviating symptoms associated with ischemic heart conditions. Your healthcare provider may prescribe vasodilators to manage conditions involving restricted blood flow and high blood pressure effectively.
Side Effects and Risks: Vasoconstrictors vs Vasodilators
Vasoconstrictors can cause side effects such as increased blood pressure, headaches, and risk of heart attack or stroke due to reduced blood flow. Vasodilators may lead to low blood pressure, dizziness, headaches, and potential reflex tachycardia as blood vessels widen. Both drug classes require careful monitoring in patients with cardiovascular conditions to balance therapeutic benefits against risks.
Choosing the Right Agent: Clinical Considerations and Guidelines
Choosing the right vasoconstrictor or vasodilator depends on patient-specific factors such as blood pressure status, cardiovascular health, and the underlying condition being treated. Vasoconstrictors are typically indicated in hypotensive emergencies to increase vascular resistance and improve perfusion, while vasodilators are preferred in hypertension and heart failure for reducing afterload and myocardial oxygen demand. Your healthcare provider will evaluate clinical guidelines, potential side effects, and drug interactions to optimize therapeutic outcomes safely.
Vasoconstrictor vs Vasodilator Infographic
 libmatt.com
libmatt.com