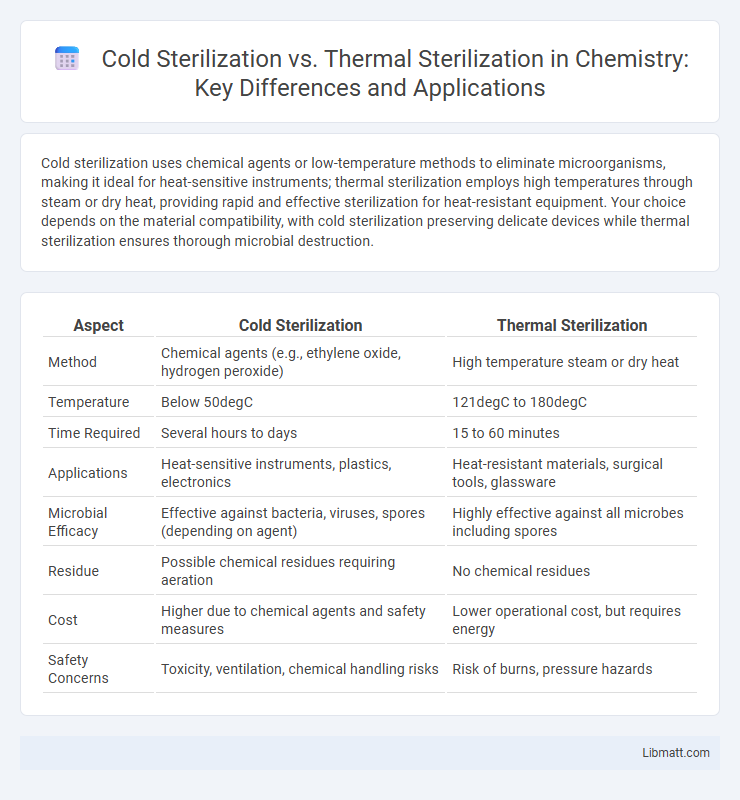
Cold sterilization uses chemical agents or low-temperature methods to eliminate microorganisms, making it ideal for heat-sensitive instruments; thermal sterilization employs high temperatures through steam or dry heat, providing rapid and effective sterilization for heat-resistant equipment. Your choice depends on the material compatibility, with cold sterilization preserving delicate devices while thermal sterilization ensures thorough microbial destruction.
Table of Comparison
| Aspect | Cold Sterilization | Thermal Sterilization |
|---|---|---|
| Method | Chemical agents (e.g., ethylene oxide, hydrogen peroxide) | High temperature steam or dry heat |
| Temperature | Below 50degC | 121degC to 180degC |
| Time Required | Several hours to days | 15 to 60 minutes |
| Applications | Heat-sensitive instruments, plastics, electronics | Heat-resistant materials, surgical tools, glassware |
| Microbial Efficacy | Effective against bacteria, viruses, spores (depending on agent) | Highly effective against all microbes including spores |
| Residue | Possible chemical residues requiring aeration | No chemical residues |
| Cost | Higher due to chemical agents and safety measures | Lower operational cost, but requires energy |
| Safety Concerns | Toxicity, ventilation, chemical handling risks | Risk of burns, pressure hazards |
Introduction to Sterilization Methods
Cold sterilization employs chemical agents like ethylene oxide, hydrogen peroxide, or peracetic acid to eliminate microorganisms at low temperatures, preserving heat-sensitive equipment. Thermal sterilization relies on moist heat, such as autoclaving at 121degC for 15-30 minutes, to denature proteins and destroy microbial life effectively. Selection between these methods depends on material compatibility, sterilization time, and microbial resistance profiles.
Definition of Cold Sterilization
Cold sterilization refers to a sterilization process using chemical agents at low temperatures to eliminate microorganisms without heat exposure, commonly employed for heat-sensitive medical instruments and devices. This method utilizes chemicals such as ethylene oxide, hydrogen peroxide plasma, or peracetic acid to achieve microbial inactivation, ensuring sterilization without compromising the integrity of delicate materials. Cold sterilization is essential for maintaining sterility in medical environments where thermal sterilization methods like autoclaving or dry heat are unsuitable.
Definition of Thermal Sterilization
Thermal sterilization uses high temperatures, typically above 121degC, to kill microorganisms and spores in food or medical equipment by denaturing proteins and enzymes. This method includes techniques such as autoclaving, boiling, and dry heat sterilization, ensuring effective microbial destruction through controlled heat exposure. Thermal sterilization is widely favored for its reliability in eliminating pathogens, especially in heat-resistant products.
Mechanisms of Action: Cold vs Thermal Sterilization
Cold sterilization utilizes chemical agents like ethylene oxide or hydrogen peroxide vapor to disrupt microbial cell membranes, proteins, and DNA through oxidation or alkylation, effectively inactivating pathogens at low temperatures. Thermal sterilization employs high heat, either through moist heat (steam under pressure) or dry heat, to denature proteins and cause irreversible coagulation and oxidation, resulting in microbial death. Cold sterilization is ideal for heat-sensitive instruments, whereas thermal sterilization ensures reliable microbial destruction through rapid and complete thermal energy transfer.
Common Applications of Cold Sterilization
Cold sterilization is commonly applied in medical settings for heat-sensitive instruments such as endoscopes, plastic syringes, and delicate surgical tools that cannot withstand high temperatures. It is also widely used in the pharmaceutical industry to sterilize heat-labile solutions and in food processing for sterilizing liquid products without altering their taste or nutritional value. Your choice of cold sterilization methods, such as chemical disinfectants or gas sterilization, ensures effective microbial elimination without compromising material integrity.
Common Applications of Thermal Sterilization
Thermal sterilization is widely used in the food industry, particularly for canned goods, dairy products, and beverages to ensure microbial safety and extend shelf life. It is also a standard method in healthcare for sterilizing surgical instruments and medical devices, relying on high temperatures to eliminate bacteria and spores. Pharmaceutical products, including heat-resistant medications and solutions, commonly undergo thermal sterilization to maintain product integrity while achieving sterility.
Advantages of Cold Sterilization
Cold sterilization offers significant advantages, including the ability to sterilize heat-sensitive medical instruments and equipment without damage. It reduces the risk of corrosion or deformation that can occur with thermal sterilization, making it ideal for delicate devices. Furthermore, cold sterilization processes, such as plasma or chemical methods, often require less energy and shorter cycle times, enhancing operational efficiency in healthcare settings.
Advantages of Thermal Sterilization
Thermal sterilization provides rapid and effective elimination of microorganisms through high temperatures, ensuring a reliable method for sterilizing heat-resistant medical instruments and food products. It offers consistent results with minimal risk of chemical residues, making it ideal for applications where chemical exposure must be avoided. When your priority is proven efficacy and safety in sterilization, thermal methods are often preferred for their thorough microbial inactivation.
Limitations and Risks: Cold vs Thermal Sterilization
Cold sterilization techniques, such as chemical sterilants and plasma sterilization, often face limitations in penetrating dense or irregularly shaped materials and can leave toxic residues posing risks to sensitive equipment and human health. Thermal sterilization, including autoclaving and dry heat methods, effectively kills a broad spectrum of microorganisms but risks damaging heat-sensitive instruments and may cause material degradation or warping. Both methods require careful consideration of compatibility with medical devices and contaminants to balance sterilization efficacy against potential material or biological hazards.
Choosing the Right Sterilization Method
Choosing the right sterilization method depends on the heat sensitivity of the items and the required level of microbial reduction. Cold sterilization methods, such as chemical disinfectants or ozone, are ideal for heat-sensitive instruments and materials that cannot withstand high temperatures. Your selection should balance effectiveness, material compatibility, and processing time to ensure optimal sterilization outcomes.
Cold sterilization vs thermal sterilization Infographic
 libmatt.com
libmatt.com