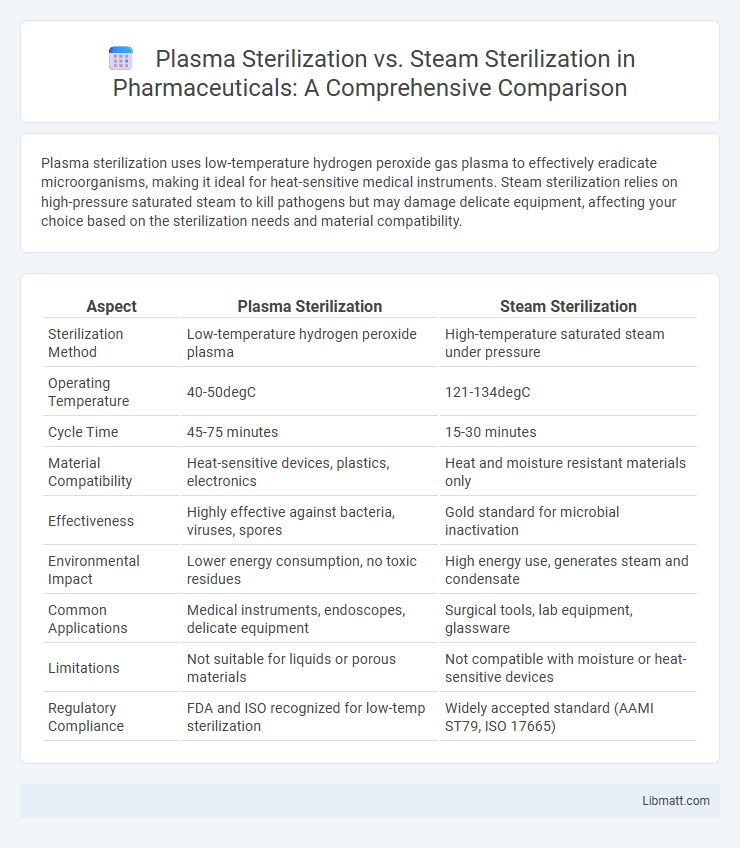
Plasma sterilization uses low-temperature hydrogen peroxide gas plasma to effectively eradicate microorganisms, making it ideal for heat-sensitive medical instruments. Steam sterilization relies on high-pressure saturated steam to kill pathogens but may damage delicate equipment, affecting your choice based on the sterilization needs and material compatibility.
Table of Comparison
| Aspect | Plasma Sterilization | Steam Sterilization |
|---|---|---|
| Sterilization Method | Low-temperature hydrogen peroxide plasma | High-temperature saturated steam under pressure |
| Operating Temperature | 40-50degC | 121-134degC |
| Cycle Time | 45-75 minutes | 15-30 minutes |
| Material Compatibility | Heat-sensitive devices, plastics, electronics | Heat and moisture resistant materials only |
| Effectiveness | Highly effective against bacteria, viruses, spores | Gold standard for microbial inactivation |
| Environmental Impact | Lower energy consumption, no toxic residues | High energy use, generates steam and condensate |
| Common Applications | Medical instruments, endoscopes, delicate equipment | Surgical tools, lab equipment, glassware |
| Limitations | Not suitable for liquids or porous materials | Not compatible with moisture or heat-sensitive devices |
| Regulatory Compliance | FDA and ISO recognized for low-temp sterilization | Widely accepted standard (AAMI ST79, ISO 17665) |
Introduction to Sterilization Methods
Plasma sterilization uses low-temperature hydrogen peroxide gas plasma to effectively eliminate microorganisms, making it ideal for heat-sensitive medical instruments. Steam sterilization employs saturated steam under pressure, offering a reliable and widely used method with rapid cycle times for heat-resistant equipment. Understanding these methods helps you select the appropriate sterilization process based on the material compatibility and sterilization requirements.
Overview of Plasma Sterilization
Plasma sterilization utilizes low-temperature hydrogen peroxide gas plasma to effectively eliminate microorganisms on heat-sensitive medical instruments, offering a rapid and residue-free sterilization process. This method generates reactive species such as free radicals and UV photons that disrupt microbial DNA and cellular structures without damaging delicate equipment. Plasma sterilization is highly suited for complex instruments, providing an efficient alternative to traditional steam sterilization that requires high heat and moisture.
Overview of Steam Sterilization
Steam sterilization, also known as autoclaving, uses saturated steam under high pressure at temperatures typically between 121degC and 134degC to effectively eliminate microorganisms, including spores. This method is widely recognized for its efficiency, speed, and ability to penetrate dense materials, making it the standard in hospitals and laboratories for sterilizing surgical instruments, glassware, and certain medical devices. However, steam sterilization is not suitable for heat-sensitive or moisture-sensitive items, which may require alternative methods such as plasma sterilization.
Mechanisms of Action: Plasma vs Steam
Plasma sterilization operates by generating reactive ionized gases that disrupt microbial cell membranes and DNA through oxidative damage and free radical formation. Steam sterilization relies on saturated steam under pressure to coagulate microbial proteins, effectively denaturing enzymes and structural components. The plasma method offers low-temperature sterilization suitable for heat-sensitive instruments, whereas steam sterilization requires high temperature and humidity to achieve microbial inactivation.
Effectiveness Against Microorganisms
Plasma sterilization uses reactive ionized gas to destroy microorganisms, offering effective sterilization for heat-sensitive instruments by efficiently killing bacteria, viruses, and spores. Steam sterilization employs high-pressure saturated steam at temperatures typically between 121-134degC, providing reliable, broad-spectrum antimicrobial activity against all forms of microorganisms including bacterial endospores. Your choice between these methods should consider the nature of the instruments and the level of microbial resistance you need to overcome for optimal infection control.
Equipment Compatibility and Material Safety
Plasma sterilization is compatible with heat- and moisture-sensitive medical devices, such as endoscopes and electronic instruments, as it uses low-temperature hydrogen peroxide gas plasma, preserving the integrity of delicate materials. Steam sterilization, operating at high temperatures and pressure, is ideal for heat-resistant instruments like surgical steel but can damage plastics, optics, and electronics. Selecting the appropriate sterilization method depends on equipment material specifications to ensure both safety and sterilization efficacy.
Cycle Duration and Efficiency
Plasma sterilization offers significantly shorter cycle durations, typically ranging from 45 to 75 minutes, compared to steam sterilization cycles that usually take 30 to 60 minutes but require longer cooling times. The low-temperature process in plasma sterilization enhances efficiency by reducing equipment wear and enabling safer sterilization of heat- and moisture-sensitive instruments. Steam sterilization remains highly effective for sterilizing heat-resistant medical devices, but plasma sterilization provides advantages in speed and compatibility with delicate materials.
Environmental Impact and Residuals
Plasma sterilization significantly reduces environmental impact by operating at lower temperatures and using non-toxic hydrogen peroxide vapor, producing minimal hazardous waste compared to steam sterilization. Steam sterilization consumes large amounts of water and energy, generating heat and moisture that can contribute to increased resource use and potential corrosion in equipment. Unlike steam sterilization, plasma sterilization leaves no toxic residuals, ensuring safer disposal and reduced ecological footprint.
Cost Comparison and Operational Considerations
Plasma sterilization generally incurs higher upfront equipment costs compared to steam sterilization but offers savings on water and energy usage, making it more cost-effective for facilities prioritizing environmental sustainability. Steam sterilization features lower initial investment and faster cycle times, suitable for high-volume settings, yet requires significant water and energy resources, impacting operational expenses. Your choice should weigh long-term utility costs and sterilization cycle efficiency against budget constraints and environmental goals.
Choosing the Right Sterilization Method
Choosing the right sterilization method depends on the type of instruments and materials involved; plasma sterilization is ideal for heat-sensitive and moisture-sensitive devices due to its low-temperature, non-corrosive process. Steam sterilization, also known as autoclaving, is highly effective for heat-resistant surgical instruments and linens, providing rapid and reliable microbial kill with saturated steam under pressure. Consider factors such as material compatibility, sterilization cycle time, and environmental impact when selecting between plasma and steam sterilization techniques.
Plasma Sterilization vs Steam Sterilization Infographic
 libmatt.com
libmatt.com