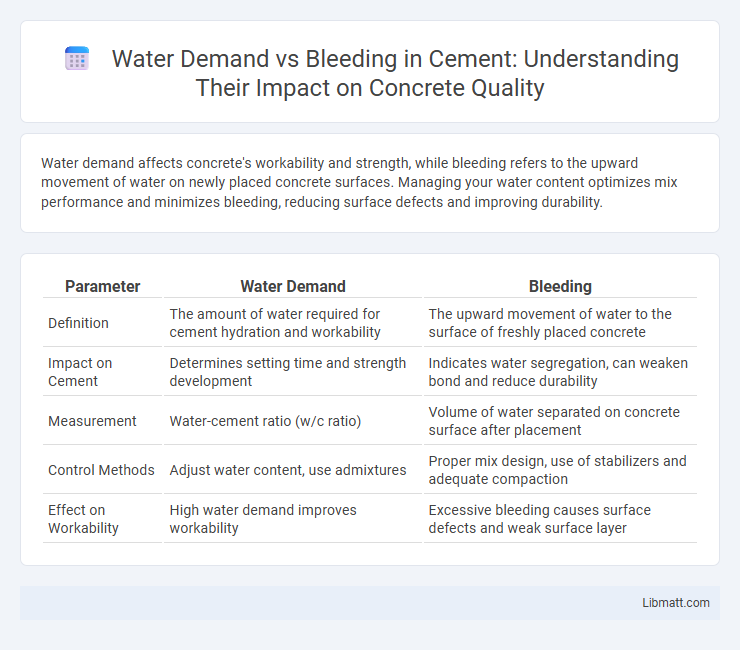
Water demand affects concrete's workability and strength, while bleeding refers to the upward movement of water on newly placed concrete surfaces. Managing your water content optimizes mix performance and minimizes bleeding, reducing surface defects and improving durability.
Table of Comparison
| Parameter | Water Demand | Bleeding |
|---|---|---|
| Definition | The amount of water required for cement hydration and workability | The upward movement of water to the surface of freshly placed concrete |
| Impact on Cement | Determines setting time and strength development | Indicates water segregation, can weaken bond and reduce durability |
| Measurement | Water-cement ratio (w/c ratio) | Volume of water separated on concrete surface after placement |
| Control Methods | Adjust water content, use admixtures | Proper mix design, use of stabilizers and adequate compaction |
| Effect on Workability | High water demand improves workability | Excessive bleeding causes surface defects and weak surface layer |
Understanding Water Demand in the Human Body
Water demand in the human body varies according to factors such as age, activity level, and climate, influencing hydration status and cellular function. Bleeding increases water demand significantly as the body loses fluids and requires replenishment to maintain blood volume and support healing processes. Proper understanding of water demand during bleeding is crucial for effective fluid replacement therapy and preventing dehydration-related complications.
The Role of Water in Blood Volume Regulation
Water plays a critical role in regulating blood volume by maintaining the balance between water demand and bleeding. When bleeding occurs, water shifts from the interstitial and intracellular spaces into the bloodstream to compensate for the volume loss and sustain adequate circulation. Proper hydration ensures your body can effectively manage blood volume and support cardiovascular stability during hemorrhagic events.
Causes and Mechanisms of Bleeding
Bleeding in concrete occurs when excess water rises to the surface after the initial placement, primarily caused by the settlement of solid particles and insufficient particle packing. High water demand increases bleeding by enlarging capillary channels, which facilitates water migration and reduces uniform hydration. The mechanism involves gravitational settling and pressure differences within the fresh mix, creating channels that compromise surface durability and contribute to segregation.
How Bleeding Impacts Body Water Needs
Bleeding increases your body's water demand by causing a direct loss of fluids alongside blood, leading to dehydration risk if not promptly managed. The fluid volume lost through bleeding must be replenished to maintain adequate blood pressure and ensure proper circulation. Proper hydration supports the body's ability to compensate for fluid loss and aids in the healing process.
Dehydration Risks During Hemorrhage
Water demand increases significantly during hemorrhage as the body attempts to maintain blood volume and pressure, heightening the risk of dehydration. Inadequate hydration exacerbates hypovolemia, impairs tissue perfusion, and can lead to organ failure. Effective management of bleeding requires careful monitoring of fluid balance to prevent dehydration and support hemodynamic stability.
Water Intake Recommendations After Blood Loss
Maintaining proper hydration is critical after blood loss to support blood volume restoration and promote healing. Experts recommend consuming at least 2 to 3 liters of water daily, tailored to your body weight and activity level, to compensate for fluid loss. Monitoring your water intake closely ensures effective recovery and prevents dehydration complications.
Signs of Fluid Deficiency Following Bleeding Events
Signs of fluid deficiency following bleeding events include rapid heart rate, low blood pressure, dizziness, and decreased urine output, indicating the body's struggle to maintain adequate hydration and circulatory volume. Increased water demand after bleeding is critical to restore plasma volume and prevent hypovolemic shock, emphasizing the importance of prompt fluid replacement. Monitoring these clinical signs alongside laboratory indicators such as elevated hematocrit and lactate levels aids in timely detection and management of fluid deficiency.
Medical Interventions: Rehydration and Blood Replacement
Effective management of water demand versus bleeding in medical interventions involves rapid rehydration through intravenous fluids to restore circulatory volume and prevent hypovolemic shock. Blood replacement therapies using packed red blood cells or whole blood transfusions are critical to restore oxygen-carrying capacity and maintain tissue perfusion. Precise monitoring of electrolyte balance, hemoglobin levels, and vital signs ensures optimized fluid resuscitation and blood transfusion tailored to patient needs.
Managing Fluid Balance in Trauma and Surgery
Effective management of water demand versus bleeding is crucial in trauma and surgery to maintain optimal fluid balance and ensure tissue perfusion. Rigid monitoring of blood loss alongside tailored intravenous fluid replacement helps prevent complications such as hypovolemia or fluid overload. Your care team must continuously assess hemodynamic parameters to customize fluid therapy, enhancing recovery and reducing morbidity.
Preventing Complications: Restoring Water and Blood Equilibrium
Balancing water demand and bleeding is critical in preventing complications during medical treatment or trauma care. Restoring equilibrium between hydration and blood volume helps maintain optimal cardiovascular function and tissue perfusion, reducing risks of shock or organ failure. Your proactive management of fluid replacement and bleeding control ensures faster recovery and improved patient outcomes.
Water demand vs Bleeding Infographic
 libmatt.com
libmatt.com